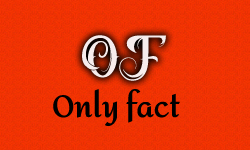
Prime Minister Narendra Modi’s ambitious Ayushman Bharat Yojana has been a hot topic of discussion across social media and mainstream media. Among the many claims being circulated, one particularly striking allegation is that a fraud or scam worth ₹562 crore has occurred within the scheme. Some social media users claim that while the total budget of Ayushman Bharat Yojana is ₹7,000 crore, a scam of ₹500 crore has already taken place. As a result, they argue that the health insurance scheme is nothing more than a complete scam.
Arun Arora posted, ‘Total budget 7000 crore. Fraud 562 crores. Ayushman yojna is a scam’
Total budget 7000 crore
— Arun Arora (@Arun2981) February 12, 2025
Fraud 562 crores
Ayushman yojna is a scam https://t.co/cFV5czgIip
Nitin shared, ‘Total budget 7000 crore, Fraud 562 crores Ayushman yojna is a scam.’
Total budget 7000 crore Fraud 562 crores Ayushman yojna is a scam pic.twitter.com/XkWWnBynsR
— ηᎥ†Ꭵղ (@nkk_123) February 13, 2025
Punjab Kesari wrote, ‘Big disclosure of fraud in Ayushman Bharat Yojana, 2.7 lakh claims worth Rs 562 crore found to be fake.’
Ayushman Bharat Yojana में फर्जीवाड़े का बड़ा खुलासा, 562 करोड़ रुपये के 2.7 लाख क्लेम पाए गए फर्जी#Modigovt #AyushmanBharatYojana #Fraud #NationalAntiFraudUnit #Privatehospitals #562crorerupees #2.7lakhfakeclaimshttps://t.co/JTuwGwxNCn
— Punjab Kesari (@punjabkesari) February 12, 2025
Guramneet Singh Mangal, Utkarsh and Gulrose views shared a similar claim.
Also Read: PM Modi’s AI Observation Proven Right: Fact-Check Confirms Bias in AI-Generated Images
Fact Check
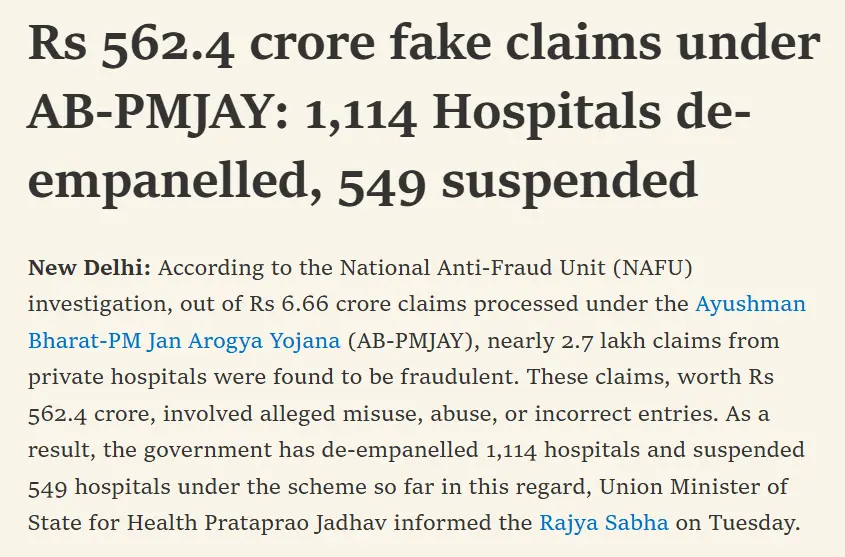
To investigate this matter, we conducted a Google search and found a relevant article published on Medical Dialogue on February 14, 2025. According to the report, a National Anti-Fraud Unit (NAFU) investigation revealed that out of ₹6.66 crore claims processed under the Ayushman Bharat-PM Jan Arogya Yojana (AB-PMJAY), nearly 2.7 lakh claims from private hospitals were identified as fraudulent. These claims, worth ₹562.4 crore, involved suspected misuse, abuse, or incorrect entries. Consequently, the government has taken strict action, de-empaneling 1,114 hospitals and suspending 549 hospitals under the scheme, as informed by Union Minister of State for Health, Prataprao Jadhav, in the Rajya Sabha.
The report further added that, to prevent and mitigate such fraudulent activities, the government has implemented AI-driven monitoring and real-time tracking systems. If any hospital is suspected of engaging in fraudulent billing, NAFU thoroughly examines the claims and places them on hold until proper verification is conducted, the minister added.
Additionally, we found a question posed in the Rajya Sabha by RJD MP Shri A.D. Singh. He inquired whether private hospitals had engaged in fraudulent billing under Ayushman Bharat-PM Jan Arogya Yojana (AB-PMJAY), thereby exploiting vulnerable patients. He also sought details regarding the state-wise and hospital-wise instances of such fraud, the actions taken against hospitals submitting fake claims, and the measures being considered to prevent the misuse of public funds under the scheme.
In response, Minister of State for Health and Family Welfare, Shri Prataprao Jadhav, emphasized that ‘AB-PMJAY is a flagship government initiative providing health coverage of ₹5 lakh per family per year for secondary and tertiary care hospitalization. The scheme benefits approximately 55 crore people from 12.37 crore economically vulnerable families, constituting the bottom 40% of India’s population. Recently, its coverage was expanded to include 6 crore senior citizens aged 70 and above from 4.5 crore families, irrespective of socio-economic status, through the Vay Vandana Card.’
The minister further added, ‘The government’s zero-tolerance policy toward fraud and abuse within the scheme. Various measures are in place to prevent, detect, and deter fraudulent activities at different stages of implementation. NAFU, operating under the National Health Authority (NHA), collaborates with State Anti-Fraud Units (SAFU) to investigate and address fraudulent claims. From the 6.66 crore claims processed by NAFU, 2.7 lakh claims from private hospitals, totaling ₹562.4 crore, were flagged due to suspected misuse, abuse, or incorrect entries. Suspicious claims from empaneled hospitals are withheld until a thorough verification process, including field investigations by SAFU teams, is completed.’
‘To address such malpractice, NHA has issued stringent guidelines, including suspending, blacklisting, or de-empaneling hospitals found guilty of fraud. Fraudulent claims are rejected, and penalties or legal action are imposed on violators. Advanced AI-based systems facilitate real-time monitoring of hospital claims, while random audits and surprise inspections ensure the authenticity of claims. State Health Agencies (SHAs) also conduct routine desk and field medical audits. As a result of these strict measures, 1,114 hospitals have been de-empaneled, and 549 hospitals have been suspended’.
The government’s response clarifies that 2.7 lakh claims worth ₹562.4 crore were deemed “non-admissible” and subsequently withheld for further scrutiny. This means that while private hospitals attempted to defraud the government by submitting false claims, no payments were made against these claims. Therefore, there was no scam or financial loss to the government.
Furthermore, the National Anti-Fraud Unit (NAFU) has deployed 57 different fraud-detection technologies to identify suspicious claims before disbursing payments. These technologies include rule-based triggers, machine learning algorithms, fuzzy logic, image classification, and data de-duplication. Other security measures, such as enhanced access controls for NHA’s IT system, real-time dashboards highlighting suspicious cases, routine database monitoring, and data analytics techniques, have also been implemented.
The government’s firm stance and proactive measures have successfully prevented fraudulent claims from being processed, ensuring no loss to the public exchequer. Instead, the attempted fraud was detected and thwarted, leading to the removal and suspension of numerous hospitals as a punitive measure.
| Claim | Rs 562 crore scam in Ayushman Bharat Yojana |
| Claimed by | Social media users |
| Fact Check | There is no ₹562 crore scam in Ayushman Bharat-PMJAY. The government identified fraudulent claims before disbursing funds, effectively stopping payments on fake claims. Additionally, strict action was taken by de-empaneling 1,114 hospitals and suspending 549 others. |
Also Read: Edited Image Falsely Shows PM Modi Traveling in a Taxi in France